November 14th is World Diabetes Day. While diabetes is not a certain outcome of PWS, it is not uncommon for individuals with PWS to develop it over time. People with PWS may be at higher risk due to a combination of metabolic and hormonal differences that affect how their bodies use energy and manage blood sugar.
Those who are overweight have an even greater risk, but the good news is that with balanced nutrition, regular physical activity, ongoing monitoring, and early interventions, individuals can lower their chances of developing diabetes and lessen its impact if it does occur.
If you are concerned about diabetes, the most important first step is to speak with your loved one’s healthcare provider. Together, you can create a plan for prevention and wellness.
What is Diabetes?
The American Diabetes Association (ADA) defines diabetes as a chronic condition where the body’s blood glucose (blood sugar) is too high, resulting from the body’s inability to properly use or store it for energy.
There are multiple types of diabetes, with Type 1 and Type 2 as the most common.
Type 1 Diabetes
This is an autoimmune condition and is not caused by diet or lifestyle. It usually begins in childhood and occurs when the body can’t make its own insulin or produces very little. People with Type 1 diabetes must take insulin to manage their blood sugar levels.
Type 2 Diabetes
In this form, the body can still make insulin but doesn’t use it properly. Over time, this leads to higher blood sugar levels. Type 2 diabetes is the most common form of diabetes seen in individuals with PWS.
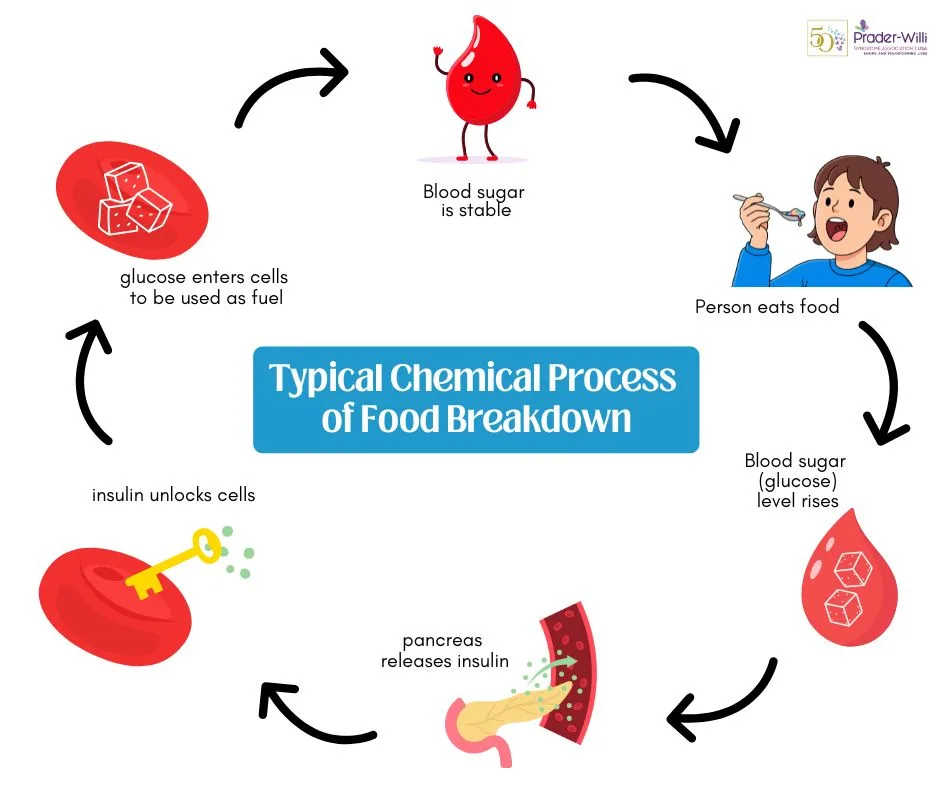
How is food broken down?
In a person without diabetes: When a person eats, the food is broken down into glucose (sugar), which enters the bloodstream. As blood sugar levels rise, the pancreas releases insulin. Insulin acts like a key, unlocking the body’s cells so glucose can move inside and be used as fuel. Once the cells absorb the glucose, blood sugar levels return to a healthy, stable range
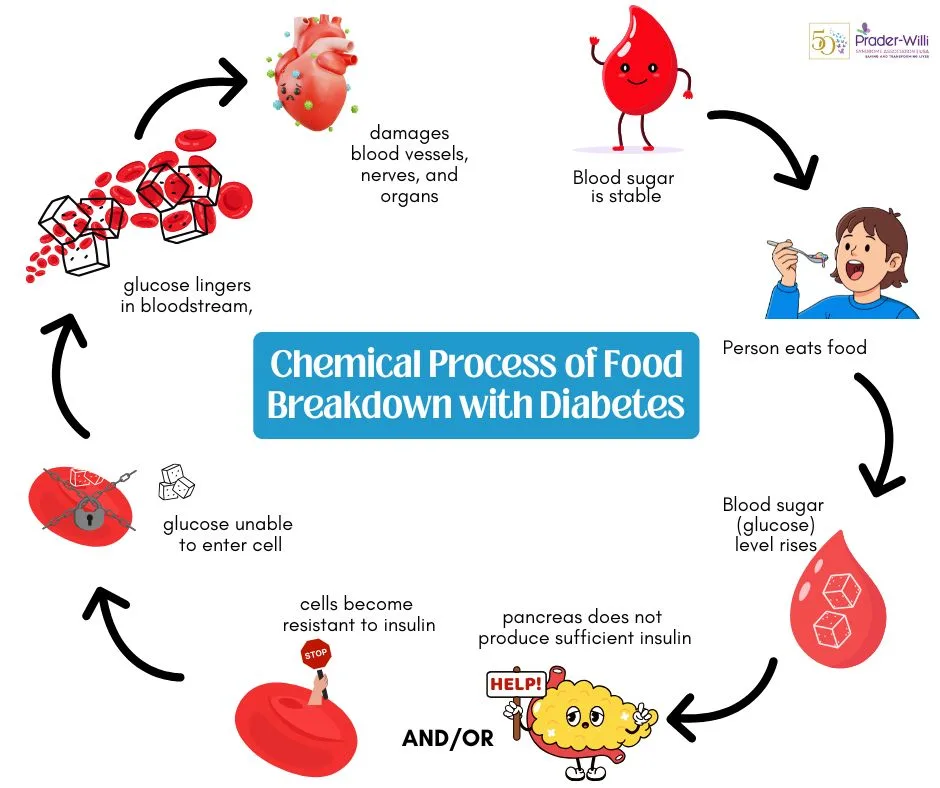
In a person with diabetes:
The process doesn’t work as it should. The pancreas may not make enough insulin, or the body’s cells may become resistant to it. Sometimes both happen. As a result, glucose cannot enter the cells and instead stays in the bloodstream. Over time, high levels of glucose in the blood can damage blood vessels, nerves, and organs.
Prevention strategies include:
Regular physical activity: Encourage daily movement suited to the person’s ability level (e.g., walks, swimming, dancing, or adaptive fitness). Even short, consistent activity helps the body use insulin more effectively.
Balanced, portion-controlled meals: Follow a structured meal plan designed for PWS.
Consistent sleep routines: Quality sleep supports healthy hormone regulation and can improve metabolism and mood.
Routine medical monitoring: Work closely with your healthcare provider to monitor weight, fasting glucose, and HbA1c (average blood sugar levels). Regular bloodwork helps detect early changes, so adjustments can be made before diabetes develops.
Medication and hormone management: Review growth hormone and other medications regularly with your endocrinologist, as these can affect body composition, metabolism, and insulin sensitivity.
What are some symptoms to look for?
Excessive thirst
Excessive urination
Fatigue
Blurred vision
Numbness or tingling in hands and feet
Resources:
What is Diabetes? Types, Symptoms, and Causes – Harvard Health
Share this!


 Perry A. Zirkel has written more than 1,500 publications on various aspects of school law, with an emphasis on legal issues in special education. He writes a regular column for NAESP’s Principal magazine and NASP’s Communiqué newsletter, and he did so previously for Phi Delta Kappan and Teaching Exceptional Children.
Perry A. Zirkel has written more than 1,500 publications on various aspects of school law, with an emphasis on legal issues in special education. He writes a regular column for NAESP’s Principal magazine and NASP’s Communiqué newsletter, and he did so previously for Phi Delta Kappan and Teaching Exceptional Children. Jennifer Bolander has been serving as a Special Education Specialist for PWSA (USA) since October of 2015. She is a graduate of John Carroll University and lives in Ohio with her husband Brad and daughters Kate (17), and Sophia (13) who was born with PWS.
Jennifer Bolander has been serving as a Special Education Specialist for PWSA (USA) since October of 2015. She is a graduate of John Carroll University and lives in Ohio with her husband Brad and daughters Kate (17), and Sophia (13) who was born with PWS. Dr. Amy McTighe is the PWS Program Manager and Inpatient Teacher at the Center for Prader-Willi Syndrome at the Children’s Institute of Pittsburgh. She graduated from Duquesne University receiving her Bachelor’s and Master’s degree in Education with a focus on elementary education, special education, and language arts.
Dr. Amy McTighe is the PWS Program Manager and Inpatient Teacher at the Center for Prader-Willi Syndrome at the Children’s Institute of Pittsburgh. She graduated from Duquesne University receiving her Bachelor’s and Master’s degree in Education with a focus on elementary education, special education, and language arts. Evan has worked with the Prader-Willi Syndrome Association (USA) since 2007 primarily as a Crisis Intervention and Family Support Counselor. Evans works with parents and schools to foster strong collaborative relationships and appropriate educational environments for students with PWS.
Evan has worked with the Prader-Willi Syndrome Association (USA) since 2007 primarily as a Crisis Intervention and Family Support Counselor. Evans works with parents and schools to foster strong collaborative relationships and appropriate educational environments for students with PWS. Staci Zimmerman works for Prader-Willi Syndrome Association of Colorado as an Individualized Education Program (IEP) consultant. Staci collaborates with the PWS multi-disciplinary clinic at the Children’s Hospital in Denver supporting families and school districts around the United States with their child’s Individual Educational Plan.
Staci Zimmerman works for Prader-Willi Syndrome Association of Colorado as an Individualized Education Program (IEP) consultant. Staci collaborates with the PWS multi-disciplinary clinic at the Children’s Hospital in Denver supporting families and school districts around the United States with their child’s Individual Educational Plan. Founded in 2001, SDLC is a non-profit legal services organization dedicated to protecting and advancing the legal rights of people with disabilities throughout the South. It partners with the Southern Poverty Law Center, Protection and Advocacy (P&A) programs, Legal Services Corporations (LSC) and disability organizations on major, systemic disability rights issues involving the Individuals with Disabilities Education Act (IDEA), Americans with Disabilities Act (ADA), and the federal Medicaid Act. Recently in November 2014, Jim retired.
Founded in 2001, SDLC is a non-profit legal services organization dedicated to protecting and advancing the legal rights of people with disabilities throughout the South. It partners with the Southern Poverty Law Center, Protection and Advocacy (P&A) programs, Legal Services Corporations (LSC) and disability organizations on major, systemic disability rights issues involving the Individuals with Disabilities Education Act (IDEA), Americans with Disabilities Act (ADA), and the federal Medicaid Act. Recently in November 2014, Jim retired.