What Is Prader-Willi Syndrome (PWS)?
Prader-Willi syndrome affects 350,000 people worldwide.
Prader-Willi Syndrome Characteristics:
Prader-Willi syndrome (PWS) is a rare genetic disorder characterized by chronic hunger, growth hormone deficiency, and behavior challenges.
Key features include:
- Insatiable Hunger: A distinctive trait of PWS is an unending appetite. This, paired with a slowed metabolism, often leads to significant weight challenges.
- Muscle & Growth: Individuals with Prader-Willi syndrome typically have weak muscle tone and less muscle mass. They also often grow to be shorter than average if they don’t receive the right treatment.
- Cognitive Aspects: People with PWS can face learning disabilities, making everyday tasks a bit tougher.
- Behavioral Challenges: People with Prader-Willi syndrome often face various behavioral challenges. These can include frequent temper tantrums, compulsive skin picking, stubbornness, and obsessive-compulsive behaviors. Managing these behaviors requires patience and understanding.
Understanding PWS is crucial for supporting those affected, enhancing their lives, and promoting inclusivity in society.

Prader Willi Syndrome Symptoms
Early Life
Immediately after birth, the symptoms of Prader-Willi syndrome become noticeable. Infants often exhibit distinct physical and behavioral patterns.
- Muscle Weakness: Decreased muscle tone, making infants appear “floppy.”
- Feeding Difficulties: Trouble sucking or feeding, often requiring special assistance.
- Distinct Facial Features: Almond-shaped eyes and a narrow bifrontal diameter.


Childhood
The toddler and childhood years see a shift in PWS symptoms. Key challenges emerge related to eating, learning, and behavior.
- Insatiable Hunger: Beginning around age 8, leading to weight gain if not managed.
- Learning Challenges: Mild to moderate intellectual impairment and delayed motor skills.
- Behavioral Issues: Including temper tantrums, stubbornness, and compulsive behaviors.
Teenage Years
The teenage phase is challenging, especially for individuals with PWS. They have to navigate through typical growth issues unique to PWS.
- Incomplete Puberty: Delayed or incomplete physical development, which can lead to short stature.
- Social Struggles: Difficulty with peer relationships and social integration.
- Ongoing Hunger: Preventing obesity is important for people with PWS.


Adulthood
As individuals with PWS transition from young adults into adulthood, they face a blend of health and social concerns. The emphasis is often on long-term health management and social integration.
- Endocrine Issues: Challenges like diabetes or low sex hormone levels.
- Orthopedic Problems: Scoliosis and osteoporosis may develop.
- Mental Health Concerns: Risk of depression, anxiety, and other mood disorders.
Background & History of Prader-Willi Syndrome
1956
Discovery
Swiss doctors Andrea Prader, Alexis Labhart, and Heinrich Willi first identify PWS. They describe distinct symptoms like obesity and cognitive challenges in affected children.
1981
Genetic Link
Researchers find a missing part on the 15th chromosome, confirming that PWS is a genetic disorder.
1990s
Advancements in Diagnosis
New genetic testing methods emerge, allowing for earlier and more precise diagnosis. This emphasizes the critical nature of early intervention.
2000s
Global Collaboration
Medical communities worldwide collaborate, sharing knowledge, improving treatments, and supporting individuals with PWS.
Today
Advancements in Diagnosis
Innovative genetic testing methods are emerging, paving the way for earlier and more precise diagnoses. Also, many clinical trials are exploring new, proactive treatment strategies for individuals living with PWS.
Hope for the future
Prader-Willi Syndrome Clinical Trials
New trials for people with Prader-Willi syndrome show promise, giving hope to affected families and patients. This research breakthrough could lead to new treatments that greatly improve the lives of people with PWS.

Frequently Asked Questions about PWS
Prader-Willi syndrome (PWS) is a variable and complex genetic disorder resulting from an abnormality on the 15th chromosome. It occurs in males and females equally and in all races. Prevalence estimates range from 1:15,000 to 1:25,000.
Experts believe that PWS is a multistage disorder characterized by decreased fetal movement during pregnancy and low birth weight. As toddlers get older, they start gaining more weight. If we don't limit their calories, this can lead to excessive eating (hyperphagia) and obesity.
Obesity, hypotonia, and hypothalamic dysfunction are the main medical problems related to Prader-Willi syndrome. Other factors may include adverse reactions to medications, high pain tolerance, gastrointestinal and respiratory issues, lack of vomiting, and unstable temperature. Adrenal insufficiency may also occur. The main problem for people with this condition is extreme hunger, which can cause dangerous obesity.
Abnormalities on chromosome 15 cause Prader-Willi Syndrome (PWS). This happens 3 different ways:
- Gene Deletion: In many cases, critical genes on a portion of the father's chromosome 15 are missing. This is the most common cause.
- Uniparental Disomy: The child has two copies of chromosome 15 from the mother instead of one from each parent.
- Imprinting Mutation: In less than 3% of cases, there is an imprinting mutation on the father's chromosome 15. The genetic material is there but remains inactive.
PWS varies from person to person but commonly affects the brain, particularly the hypothalamus. This leads to symptoms like:
- Weak muscle tone (hypotonia) from birth.
- Poor sucking in babies, causing feeding difficulties.
- Swallowing problems with saliva and food.
- Overeating (hyperphagia) due to the brain not signaling fullness, potentially causing severe obesity. This starts between 2-4 years old.
- Short height if not treated with growth hormones.
- Bone issues like hip dysplasia and osteoporosis.
- Delayed sexual development.
- Learning difficulties and developmental delays.
- Frequent behavior problems.
- Sensitivity to certain medications.
- High pain tolerance, possibly missing injuries like fractures.
- Digestive problems, including constipation and rare cases of stomach issues after binge eating.
- Breathing problems during sleep, like sleep apnea.
- Trouble regulating body temperature.
Doctors use unique genetic tests that analyze blood and saliva to identify PWS. These tests can be costly as they require specialized lab processing.
The best first test is DNA Methylation Testing, which detects over 99% of PWS cases and checks for all three genetic subtypes. The FISH test is useful but can't identify all subtypes, so it's not the preferred initial test. Chromosome Microarray testing is also effective, especially for detecting chromosome deletions and uniparental disomy (UPD).
Prader-Willi Syndrome (PWS) usually doesn't run in families. It happens because some genes on chromosome 15 aren't working right. This happens if a part of chromosome 15 from the father is missing. It can also occur when the child gets two chromosome 15s from the mother or if the genes from both parents aren't working right.
Scientists are always looking for new ways to treat the syndrome so children and adults can have a better quality of life. However, at this time there is no cure for Prader-Willi syndrome.
In 2000, the Federal Drug Administration approved Human Growth Hormone (HGH) for patients with Prader-Willi Syndrome (PWS). Studies show that HGH offers several benefits. It not only helps increase height and reduce body fat, but also boosts stamina and bone mineral density.
Many individuals with the syndrome participate in a variety of therapies, including physical, occupational, and speech therapies.
How PWSA | USA Supports the PWS Community
Stay up to Date with PWS News
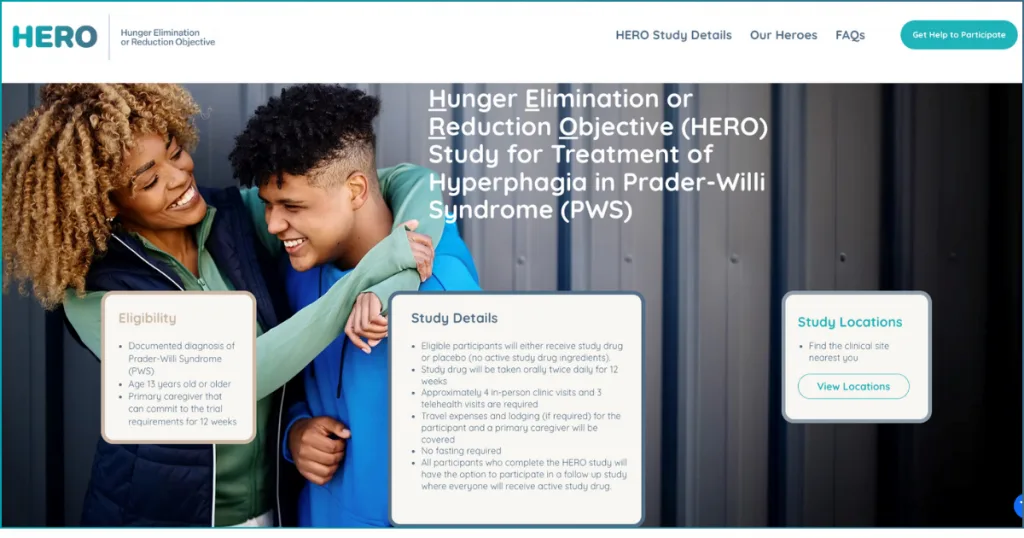
Aardvark Therapeutics HERO Trial: U.S. Sites Now Open
Aardvark Therapeutics recently launched HERO, a global Phase 3 clinical trial investigating ARD-101, an innovative, orally administered treatment designed to help reduce hyperphagia (excessive hunger) and food-seeking behaviors in individuals with Prader-Willi syndrome (PWS). This randomized, double-blind, placebo-controlled trial is an important step toward identifying a potential new treatment option for the PWS community, and […]
Aardvark Therapeutics Launches HERO, A Phase 3 Trial of ARD-101 for Treatment of Hyperphagia in PWS; Now Enrolling Participants in the US
Aardvark Therapeutics recently launched HERO, a global Phase 3 randomized, double-blind, placebo-controlled clinical trial of ARD-101. ARD-101 is a novel, orally administered investigational therapy being studied to see if it can reduce excessive hunger and food-seeking behaviors in individuals with PWS. About the HERO Trial As part of the HERO study, participants will be randomly […]
Unlocking a New Path to Treat Hyperphagia in PWS: A Conversation with Aardvark Therapeutics
Hyperphagia, the relentless hunger that those living with Prader-Willi syndrome (PWS) experience, remains one of the most challenging and life-altering symptoms for individuals and families. But a promising investigational drug called ARD-101 is offering hope. In our April 29th episode of PWS United, Aardvark Therapeutics’ Dr. Tien Lee, M.D., CEO and Founder, and Dr. Manasi […]


 Jennifer Bolander has been serving as a Special Education Specialist for PWSA (USA) since October of 2015. She is a graduate of John Carroll University and lives in Ohio with her husband Brad and daughters Kate (17), and Sophia (13) who was born with PWS.
Jennifer Bolander has been serving as a Special Education Specialist for PWSA (USA) since October of 2015. She is a graduate of John Carroll University and lives in Ohio with her husband Brad and daughters Kate (17), and Sophia (13) who was born with PWS. Perry A. Zirkel has written more than 1,500 publications on various aspects of school law, with an emphasis on legal issues in special education. He writes a regular column for NAESP’s Principal magazine and NASP’s Communiqué newsletter, and he did so previously for Phi Delta Kappan and Teaching Exceptional Children.
Perry A. Zirkel has written more than 1,500 publications on various aspects of school law, with an emphasis on legal issues in special education. He writes a regular column for NAESP’s Principal magazine and NASP’s Communiqué newsletter, and he did so previously for Phi Delta Kappan and Teaching Exceptional Children. Evan has worked with the Prader-Willi Syndrome Association (USA) since 2007 primarily as a Crisis Intervention and Family Support Counselor. Evans works with parents and schools to foster strong collaborative relationships and appropriate educational environments for students with PWS.
Evan has worked with the Prader-Willi Syndrome Association (USA) since 2007 primarily as a Crisis Intervention and Family Support Counselor. Evans works with parents and schools to foster strong collaborative relationships and appropriate educational environments for students with PWS. Dr. Amy McTighe is the PWS Program Manager and Inpatient Teacher at the Center for Prader-Willi Syndrome at the Children’s Institute of Pittsburgh. She graduated from Duquesne University receiving her Bachelor’s and Master’s degree in Education with a focus on elementary education, special education, and language arts.
Dr. Amy McTighe is the PWS Program Manager and Inpatient Teacher at the Center for Prader-Willi Syndrome at the Children’s Institute of Pittsburgh. She graduated from Duquesne University receiving her Bachelor’s and Master’s degree in Education with a focus on elementary education, special education, and language arts. Staci Zimmerman works for Prader-Willi Syndrome Association of Colorado as an Individualized Education Program (IEP) consultant. Staci collaborates with the PWS multi-disciplinary clinic at the Children’s Hospital in Denver supporting families and school districts around the United States with their child’s Individual Educational Plan.
Staci Zimmerman works for Prader-Willi Syndrome Association of Colorado as an Individualized Education Program (IEP) consultant. Staci collaborates with the PWS multi-disciplinary clinic at the Children’s Hospital in Denver supporting families and school districts around the United States with their child’s Individual Educational Plan. Founded in 2001, SDLC is a non-profit legal services organization dedicated to protecting and advancing the legal rights of people with disabilities throughout the South. It partners with the Southern Poverty Law Center, Protection and Advocacy (P&A) programs, Legal Services Corporations (LSC) and disability organizations on major, systemic disability rights issues involving the Individuals with Disabilities Education Act (IDEA), Americans with Disabilities Act (ADA), and the federal Medicaid Act. Recently in November 2014, Jim retired.
Founded in 2001, SDLC is a non-profit legal services organization dedicated to protecting and advancing the legal rights of people with disabilities throughout the South. It partners with the Southern Poverty Law Center, Protection and Advocacy (P&A) programs, Legal Services Corporations (LSC) and disability organizations on major, systemic disability rights issues involving the Individuals with Disabilities Education Act (IDEA), Americans with Disabilities Act (ADA), and the federal Medicaid Act. Recently in November 2014, Jim retired.