Despite our growing understanding and knowledge of the management of Prader-Willi syndrome (PWS), there are still persons with PWS who experience life-threatening complications due to obesity; and others who require inpatient treatment for severe, challenging behaviors. There are a handful of professionals who became experts in caring for these individuals at a time when they were very ill, either physically or behaviorally. For many, it was probably the most stressful time in their lives. Because of their experiences, these pioneers helped us learn about the seriousness of such health emergencies and the urgency in preventing and treating problems before they become fatal. Most of these professionals conducted research, wrote papers and shared their knowledge with other professionals who cared for persons with PWS from around the world. We have highlighted just some of the team members who have given so much to the world of PWS. We are truly grateful for their focus on those who truly needed their expertise.
In the early 1980s, Lota Mitchell, a parent of young woman with PWS, as well as a board member of PWSA l USA, was interested in starting a support group for parents connected to a medical facility, The Rehabilitation Institute (TRI) in Pittsburgh. After meeting with medical and other staff to discuss this, they agreed to start by sponsoring a 4-week summer camp. That first summer, seven kids with PWS, ages 8-12 years, attended. It went so well, the next summer another session was added for persons 13-18 years in age. The focus however gradually changed to crisis, as some of the campers were admitted to TRI outside of the summer program. By the early 1990s, the program was year-round and the term “camp” was dropped. A 7-bed unit was opened which devoted its care to persons with PWS who were experiencing life-threatening health emergencies as well as psychiatric crises. It soon grew to 2 separate units for those under the age of 21 years and for those over the age of 21. The average stay was about 46-47 days. Some stayed longer and, on occasion, return visits occurred.
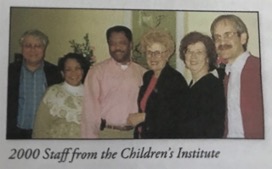
In approximately 1998, the hospital was renamed The Children’s Institute (TCI). They treated hundreds of persons with PWS from states across the USA, Canada, South Africa, Saudi Arabia and France. Most programs at TCI only treated children. However, the PWS program treated both children and adults. They utilized a multidisciplinary approach including physicians, psychologists, social workers, dieticians, speech and language therapists, occupational and physical therapists, special education teachers, program managers, team leaders and direct care personnel. They all had extensive training and experience in working with children and adults with PWS. Due to ongoing challenges with insurance coverage, the PWS inpatient program ended in 2017. TCI is continuing to offer an extension of their services in an outpatient PWS Care Coordination Program.
The first medical director for the PWS program was Dr. Anna Choraxy. Bea Maier was the senior coordinator and was put in charge of the PWS program. Bea was one of the key persons in establishing the summer camp programs for kids with PWS. She made sure the camp was a success. Youngsters lost weight, had a fun time and parents received support and education. Bea became an avid supporter and educator for not only the patients in the inpatient unit, but also faithfully attended support group meetings for parents in Pennsylvania and Ohio. Bea lost her life after a courageous battle with breast cancer.
Testimonial: Lota Mitchell, past president and board member of PWSA l USA:
“For 25 years, Bea Maier was senior coordinator with The Rehabilitation Institute of Pittsburgh, now renamed to The Children’s Institute, with many of those years devoted to PWS. I met Bea in the fall of 1980 when she was put in charge of developing a special inpatient program for PWS. She asked me to come to see her every few weeks. I thought she was looking for my “wisdom”, but I discovered my visits were really to remind her and keep her going on the project since she was an expert procrastinator.
Bea became very dedicated to PWS. She attended meetings of the local parent support group, helping with programs and providing guidance. We often traveled together for long drives and overnights to go to meetings of the Pennsylvania PWSA chapter on the eastern and central side of our very wide state where she became a board member. She attended every PWSA l USA national conference, sometimes to talk about the Rehab program, sometimes to be a presenter, and sometimes just to be there.
She probably knew as much, or more, about PWS as anyone in the country, and it was there for the asking, never pushed on anyone. She talked a lot; I think as cover for her really bad hearing.
If other parents’ experience with Bea was like mine, she was not only Rehab staff, educator and support person, but also friend. I found her to be brilliant, just a bit spacey (!), full of fascinating stories, warm and compassionate.
Her death too young from the most aggressive form of breast cancer was a real loss to everyone in the PWS world.”
One of the first physicians who provided care for persons hospitalized at TRI/TCI was Dr. Jeanne Hanchett. Dr. Hanchett graduated from Weill Cornell Medical College of Cornell University in 1961. She completed her residencies in pediatrics from Baylor College of Medicine (1961-62) and Vanderbilt University (1962-64). Dr. Jeanne has practiced pediatrics for over 60 years.
Her husband, Dr. James Hanchett, practiced internal medicine with a specialty in nephrology. He served as a consultant at TCI. He was born in Elgin, Ill. He attended Wheaton College in Illinois and medical school at Cornell University. After a residency at Vanderbilt University, he served in the Air Force during the Vietnam War and moved his family to Japan. The Hanchetts then settled in Pittsburgh. He died on September 29, 2003.
Both of these physicians contributed to our knowledge in the management of life- threatening health issues seen in persons with PWS with morbid obesity and challenging behaviors. They saw some of the most complex cases of persons experiencing severe breathing and lung complications, along with complications of diabetes and hypertension. They cared for patients who were struggling with some of the most serious complications of morbid obesity. They were frequent presenters at PWSA l USA conferences, and contributed to the second and third editions of The Management of Prader-Willi Syndrome. Dr. Jeanne Hanchett also served on the PWSA l USA Scientific Advisory board from 1992-2006.
Testimonial: Pat LaBella, parent to Beth:
“Our daughter went to The Children’s Institute in Pittsburgh, PA, in 1996 when she was 16 years old. She was there for 60 days for mental health issues and medication adjustments. At that time, TCI had a long-term care unit where all the staff was trained specifically to care for those with Prader-Willi Syndrome. While at TCI, our daughter was under the care of Dr. Jeanne Hanchett, a gentle, but firm, pediatrician dedicated to the care of and research for those with PWS.”
Another important team member in helping so many patients and families experiencing a crisis was Ken Smith. Ken started working at TRI during the summer while in school completing his degree at the University of Pittsburgh. After he graduated in 1985, he returned full time after he discovered he loved doing direct patient care. He became the assistant program coordinator, responsible for admissions. and initially worked with Bea Maier who developed the program as well as Dr. Jeanne Hanchett, the pediatrician. He became one of the team members who devoted many years to TCI and worked with many health care professionals. In 2013, after 27 years, Ken left the TCI.
In 1995, Ken was elected to serve on the PWSA l USA Board of Directors. He served many years on the board including serving as the board chair or board co-chair. After leaving TCI, he was hired as PWSA l USA executive director and served until 2017. Over the years, Ken was very devoted to providing leadership and guidance, especially in the area of crisis management. He was admired by parents, coworkers and others with whom he served.
Testimonial: Mary K. Ziccardi, Regional Director, REM Ohio, Co-chair Professional Providers Board, past member PWSA l USA Board of Directors:
“For the dozens of adults with Prader-Willi Syndrome who may have been an inpatient at The Children’s Institute or attended a PWSA conference, Ken Smith represented one of the most recognizable and friendliest faces. Through his professional roles, Ken had a unique opportunity to make friends and continue relationships with so many people, following their lives for decades. He has been able to witness some who were immobile and using oxygen to again breathe without assistance, become ambulatory and enjoy a quality of life that once was unimaginable. What set Ken apart was his ability to recall a detail about someone’s life that made them feel extraordinary, like their latest job success, volunteer experience at an animal shelter or special new friend. When the Adult Advisory Board first formed in 2003, Ken was a natural choice to be one of the inaugural leaders, providing guidance and direction to adults who wanted their voices to be heard. His calm approach and sense of humor has left an unforgettable impression on the lives of many people with Prader-Willi Syndrome over the years.”
In the early 2000s, Dr. Linda Gourash, a developmental pediatrician, became the admitting physician and treatment team leader of the PWS program at TCI. She worked almost exclusively with children and adults with PWS and related disorders. In 2005, she and Dr. Janice Forster formed the Pittsburgh Partnership, where they both served as specialists in PWS, as independent consultants. Dr. Gourash also has a private practice in developmental pediatrics in Pittsburgh.
Dr. Gourash received her medical degree from Georgetown University and completed her pediatric training at the Children’s Hospital of Pittsburgh in 1980. She served on the full-time faculty of the University of Pittsburgh School of Medicine until 1991, working primarily with developmentally disabled children hospitalized with severe behavior disorders.
Dr. Gourash has served on the PWSA | USA Clinical Advisory Board since 2004, and on the Board of Directors from 2006-2009. She contributed to the third edition of The Management of Prader-Willi Syndrome. Dr. Gourash has been a speaker at several PWSA l USA and IPWSO conferences. She, along with Dr. Forster, have frequently added a little humor and a bit of entertainment to PWSA l USA conferences. She has contributed several articles, handouts and DVDs for parents, caregivers, and professionals who seek to learn more about the health challenges faced by children and adults with PWS.
Testimonial: Lisa Graziano, former PWSA l USA Board member:
“It is without question that the PWS community has learned more about PWS behavior management strategies from Drs. Linda Gourash and Janice Forster than we’ve learned from any other professional. Indeed, only the very novice to the syndrome are not guided by their “Principles of Food Security”, now renowned worldwide for their power to reduce anxiety and improve behavior. Their seminars weave their knowledge and insights into creative, entertaining, and memorable presentations. During professional consultations they know just the right questions to ask to zero in on potential areas of behavioral intervention. Their simple mantra for medication management, “Start Slow, Go Slow”, serves as a powerful reminder to psychiatrists and other medical professionals not to overprescribe and thereby worsen the very symptoms targeted for treatment. Their collaborative research of PWS adds to our understanding and management of this complex syndrome every day. Occasionally controversial, always thought-provoking, and unceasingly caring, Linda Gourash and Janice Forster have been icons in the PWS community for well over two decades. They have taught, supported, and inspired thousands of families and professionals throughout the world. I know that what I have learned from them over the last twenty-two years has had a profound impact on how well my son is flourishing today, and I look forward to continuing to learn all they have to teach throughout the years ahead.”
Dr. Janice Forster, a Child and Adolescent Psychiatrist in private practice in Pittsburgh, PA, specializes in Developmental Neuropsychiatry. She has had over 25 years of clinical experience in the evaluation and treatment of individuals with developmental disabilities. She served as a psychiatric consultant at TCI where she evaluated over 250 individuals with PWS and has managed the severe manifestations of the disorder across all levels of care. She is also co-founder of Pittsburgh Partnership, specializing in PWS.
Dr. Forster is a graduate of the University of Pittsburgh School of Medicine (1977), and she completed her combined Pediatric Internship, Child and Adolescent Psychiatry and General Psychiatry residency through the Western Psychiatric Institute and Clinic of the University of Pittsburgh Medical Center (1982). She is a diplomat of the American Board of Psychiatry and Neurology.
Dr. Forster serves as a consultant for PWSA l USA and the International Prader-Willi Syndrome Organisation. She has presented nationally and internationally on the behavioral phenotype of PWS and psychiatric assessment and management of children and adults with the syndrome. She is also featured in a DVD produced by PWSA | USA which has recorded her presentations for more widespread distribution. She contributed to the third edition of The Management of Prader-Willi Syndrome.
Testimonial: Rob Lutz, parent and board member of PWSA l USA:
“Dr. Forster had a major impact on my daughter’s life trajectory. In her later teens, my daughter started to have significant behavioral challenges related to food and school. We tried to change all of our family/home patterns and adjust her medications but it wasn’t working. So, we went to Dr. Forster to get help and to work with our local psychiatrist. Not only was Dr. Forster fairly quickly able to make adjustments that worked, she did so compassionately and with great teamwork with our local doctors. Her comprehensive knowledge of PWS and what works medically while also tailoring to individual needs was truly impressive. We’re not sure if our daughter would be as relatively successful as she has been without Dr. Forster and her input. We also recognize that because of the antiquated rules for insurance, Dr. Forster is not compensated fully for her time. Yet she continues to give her time and effort to help families like ours. What amazing generosity!”
Dr. Greg Cherpes is a psychiatrist who also served as a consultant at TCI in the PWS program. He is board certified in child and adolescent psychiatry as well as general psychiatry. He began working on the leadership team of the PWS Behavioral Disorders Unit in 2006. During his time on staff, he provided clinical services and support to both children and adults with PWS who were experiencing psychiatric emergencies. He served on the PWSA l USA Clinical Advisory Board from 2007-2015 and PWSA l USA Board of Directors from 2009-2015. He provided psychiatric consultative services for PWSA l USA. He contributed his time to furthering the advancement of knowledge in the use of psychotropic medications in improving the quality of life for persons with PWS. He is currently in private practice in Pittsburgh, Pennsylvania.
Dr. Cherpes received his medical degree from the Medical College of Wisconsin in Milwaukee (1991). He completed his fellowship in child and adolescent psychiatry at the University of Pittsburgh Medical Center.
Testimonial: Mark Greenberg, father of Zach:
“Dr. Greg Cherpes has been a great help to the PWS community for many years. He has dedicated so much of his life to working with kids with PWS as the Director of Behavioral Health at the Center for Prader-Willi syndrome at the Children’s Institute in Pittsburgh from 2006 to 2015. While everyone with PWS has significant issues, the children who went to the Children’s Institute had special physical and mental health challenges.
As a parent whose son was at The Children’s Institute for three months I can attest to his professionalism, dedication, and thoughtfulness for our kids. We are lucky to have medical professionals such as Dr. Cherpes.”
The professionals who cared for children and adults with PWS who experienced life-threatening health situations are people who must be admired and greatly appreciated. There was always a team of people who helped these individuals improve their health. We focused on a few of these people who have given back to improving the lives of all people with PWS through their dedication and service. Unfortunately, at the current time, there are a very limited number of inpatient hospital programs that offer this level of care, specific for persons with PWS experiencing a medical or psychiatric crisis. Nexus Children’s Hospital in Texas is one of the newer programs that is caring for children with PWS who require a specialized inpatient program to address life threatening weight and behavioral health needs.







 Perry A. Zirkel has written more than 1,500 publications on various aspects of school law, with an emphasis on legal issues in special education. He writes a regular column for NAESP’s Principal magazine and NASP’s Communiqué newsletter, and he did so previously for Phi Delta Kappan and Teaching Exceptional Children.
Perry A. Zirkel has written more than 1,500 publications on various aspects of school law, with an emphasis on legal issues in special education. He writes a regular column for NAESP’s Principal magazine and NASP’s Communiqué newsletter, and he did so previously for Phi Delta Kappan and Teaching Exceptional Children. Jennifer Bolander has been serving as a Special Education Specialist for PWSA (USA) since October of 2015. She is a graduate of John Carroll University and lives in Ohio with her husband Brad and daughters Kate (17), and Sophia (13) who was born with PWS.
Jennifer Bolander has been serving as a Special Education Specialist for PWSA (USA) since October of 2015. She is a graduate of John Carroll University and lives in Ohio with her husband Brad and daughters Kate (17), and Sophia (13) who was born with PWS. Dr. Amy McTighe is the PWS Program Manager and Inpatient Teacher at the Center for Prader-Willi Syndrome at the Children’s Institute of Pittsburgh. She graduated from Duquesne University receiving her Bachelor’s and Master’s degree in Education with a focus on elementary education, special education, and language arts.
Dr. Amy McTighe is the PWS Program Manager and Inpatient Teacher at the Center for Prader-Willi Syndrome at the Children’s Institute of Pittsburgh. She graduated from Duquesne University receiving her Bachelor’s and Master’s degree in Education with a focus on elementary education, special education, and language arts. Evan has worked with the Prader-Willi Syndrome Association (USA) since 2007 primarily as a Crisis Intervention and Family Support Counselor. Evans works with parents and schools to foster strong collaborative relationships and appropriate educational environments for students with PWS.
Evan has worked with the Prader-Willi Syndrome Association (USA) since 2007 primarily as a Crisis Intervention and Family Support Counselor. Evans works with parents and schools to foster strong collaborative relationships and appropriate educational environments for students with PWS. Staci Zimmerman works for Prader-Willi Syndrome Association of Colorado as an Individualized Education Program (IEP) consultant. Staci collaborates with the PWS multi-disciplinary clinic at the Children’s Hospital in Denver supporting families and school districts around the United States with their child’s Individual Educational Plan.
Staci Zimmerman works for Prader-Willi Syndrome Association of Colorado as an Individualized Education Program (IEP) consultant. Staci collaborates with the PWS multi-disciplinary clinic at the Children’s Hospital in Denver supporting families and school districts around the United States with their child’s Individual Educational Plan. Founded in 2001, SDLC is a non-profit legal services organization dedicated to protecting and advancing the legal rights of people with disabilities throughout the South. It partners with the Southern Poverty Law Center, Protection and Advocacy (P&A) programs, Legal Services Corporations (LSC) and disability organizations on major, systemic disability rights issues involving the Individuals with Disabilities Education Act (IDEA), Americans with Disabilities Act (ADA), and the federal Medicaid Act. Recently in November 2014, Jim retired.
Founded in 2001, SDLC is a non-profit legal services organization dedicated to protecting and advancing the legal rights of people with disabilities throughout the South. It partners with the Southern Poverty Law Center, Protection and Advocacy (P&A) programs, Legal Services Corporations (LSC) and disability organizations on major, systemic disability rights issues involving the Individuals with Disabilities Education Act (IDEA), Americans with Disabilities Act (ADA), and the federal Medicaid Act. Recently in November 2014, Jim retired.