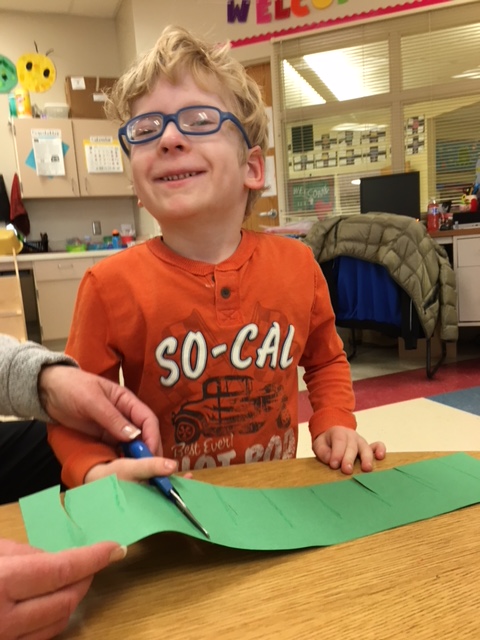
A Mother’s Experience
By Katie Moureau
My son Cade is three years old; and has been on oxygen since he was 4 months old. This year started out with a bang! One early winter morning, Cade’s pulse ox started beeping. By 5am it was alarming frequently as he was unable to maintain his oxygen levels and his heart rate had increased to over 180. He was feverish despite giving him ibuprofen. Increasing his oxygen levels to 1 liter did not change things. My husband had to clear the driveway of snow with a snow blower, so it was 7am by the time we made it to the children’s hospital emergency room. Cade was still not able to maintain normal oxygen levels and his pulse ox was dipping from 85 into the 70s while he was awake, with a high heart rate of 170-180.
Once in the ER, I requested a swab for RSV to figure out what was going on; the swab came back positive for RSV. We were then sent for X rays of his chest. He was unable to drink anything, nor maintain his oxygen levels while awake or asleep without 1.5 liters of oxygen. The doctor came in and told me that we could take him home. Thank goodness I know danger that respiratory illnesses can be for our kids with PWS. Cade was on 1.5 liters of oxygen in the ER, and our home concentrator only goes up to 1 liter. I simply looked at the doctor and stated, “I am not comfortable with that decision.” I went on to explain: “He has PWS and low tone and cannot maintain his oxygen level now, even when he is awake. We have an oxygen concentrator that only goes up to 1 liter. What happens when this gets worse? I understand this is a rare disease, and you may not know what this entails, but he needs to be monitored closely. He has not had anything to drink all night, nor can I get him to drink.”
The doctor and I then had a nice chat for about 15 minutes. We talked about PWS and what it meant for Cade. The doctor decided that admitting Cade for observation would be wise. Later a nurse came in and made a comment on how “we want to be admitted”. “Does anyone really want to be admitted?” I said calmly. The next time she came back to assess him, Cade’s oxygen had to be increased again. He is breaking out in a rash and his fever is back. Then the results from his X ray are back: Cade has lower right lobe pneumonia. The nurse then apologized immediately.
We spent the next 2 nights in the hospital on oxygen, slowly weaning him off during the day and lowering it to 1 liter at night. The good news is he’s almost back to normal oxygen needs and he is finally eating and drinking. I am so happy that PWSA-USA was able to send them information on PWS, and that I advocated for my precious baby.
How to Complain: Tips from a Medical Professional
Kathy Clark, reviewed by Dr. Dan Beaver
Even when armed with the PWSA App, the Medical Alert booklet and other publications about PWS, many parents experience the ER as a particularly unfriendly place for those with rare disorders. All medical students “learn” about PWS, but by the time they are doctors, they are left with outdated impressions of a very rare diagnosis that they never really expected to see. Most health care professionals are caring intelligent people, humbled by the things they do not know and eager to give the best care possible. There are also those who will never say, “Thanks for this booklet”, “I don’t know” or “Let me find out”. While we cannot expect every doctor, nurse, or hospital to be experts in PWS, parents should expect to be listened to and respected.
If your ER or hospital stay leaves you fuming, what can you do?
- Contact your primary care provider to let them know you are in the ER and need their support
- Ask to speak with the physician’s supervisor, for a second opinion
- Risk Management, Patient Safety, Patient Advocates, Quality Care, Patient Relations – these are different names for the department that handles complaints from patients and families. These departments take complaints very seriously. When you face a roadblock or conflict, ask for a social worker to come help you. This is a good step for several reasons: A social worker will help you communicate with the medical staff in a difficult situation and will be your advocate in filing a complaint if needed.
- Carry the Medical Alert booklet to every appointment
- Download the PWSA(USA) app and be sure you can access the booklet today – be prepared
- Don’t expect every health care professional to be fluent in PWS – be ready to educate them
- If someone does not listen, ask to speak with their supervisor or a social worker
- Call PWSA(USA) 9-5pm EST for support and coaching. We want to help you succeed!



 Jennifer Bolander has been serving as a Special Education Specialist for PWSA (USA) since October of 2015. She is a graduate of John Carroll University and lives in Ohio with her husband Brad and daughters Kate (17), and Sophia (13) who was born with PWS.
Jennifer Bolander has been serving as a Special Education Specialist for PWSA (USA) since October of 2015. She is a graduate of John Carroll University and lives in Ohio with her husband Brad and daughters Kate (17), and Sophia (13) who was born with PWS. Perry A. Zirkel has written more than 1,500 publications on various aspects of school law, with an emphasis on legal issues in special education. He writes a regular column for NAESP’s Principal magazine and NASP’s Communiqué newsletter, and he did so previously for Phi Delta Kappan and Teaching Exceptional Children.
Perry A. Zirkel has written more than 1,500 publications on various aspects of school law, with an emphasis on legal issues in special education. He writes a regular column for NAESP’s Principal magazine and NASP’s Communiqué newsletter, and he did so previously for Phi Delta Kappan and Teaching Exceptional Children. Evan has worked with the Prader-Willi Syndrome Association (USA) since 2007 primarily as a Crisis Intervention and Family Support Counselor. Evans works with parents and schools to foster strong collaborative relationships and appropriate educational environments for students with PWS.
Evan has worked with the Prader-Willi Syndrome Association (USA) since 2007 primarily as a Crisis Intervention and Family Support Counselor. Evans works with parents and schools to foster strong collaborative relationships and appropriate educational environments for students with PWS. Dr. Amy McTighe is the PWS Program Manager and Inpatient Teacher at the Center for Prader-Willi Syndrome at the Children’s Institute of Pittsburgh. She graduated from Duquesne University receiving her Bachelor’s and Master’s degree in Education with a focus on elementary education, special education, and language arts.
Dr. Amy McTighe is the PWS Program Manager and Inpatient Teacher at the Center for Prader-Willi Syndrome at the Children’s Institute of Pittsburgh. She graduated from Duquesne University receiving her Bachelor’s and Master’s degree in Education with a focus on elementary education, special education, and language arts. Staci Zimmerman works for Prader-Willi Syndrome Association of Colorado as an Individualized Education Program (IEP) consultant. Staci collaborates with the PWS multi-disciplinary clinic at the Children’s Hospital in Denver supporting families and school districts around the United States with their child’s Individual Educational Plan.
Staci Zimmerman works for Prader-Willi Syndrome Association of Colorado as an Individualized Education Program (IEP) consultant. Staci collaborates with the PWS multi-disciplinary clinic at the Children’s Hospital in Denver supporting families and school districts around the United States with their child’s Individual Educational Plan. Founded in 2001, SDLC is a non-profit legal services organization dedicated to protecting and advancing the legal rights of people with disabilities throughout the South. It partners with the Southern Poverty Law Center, Protection and Advocacy (P&A) programs, Legal Services Corporations (LSC) and disability organizations on major, systemic disability rights issues involving the Individuals with Disabilities Education Act (IDEA), Americans with Disabilities Act (ADA), and the federal Medicaid Act. Recently in November 2014, Jim retired.
Founded in 2001, SDLC is a non-profit legal services organization dedicated to protecting and advancing the legal rights of people with disabilities throughout the South. It partners with the Southern Poverty Law Center, Protection and Advocacy (P&A) programs, Legal Services Corporations (LSC) and disability organizations on major, systemic disability rights issues involving the Individuals with Disabilities Education Act (IDEA), Americans with Disabilities Act (ADA), and the federal Medicaid Act. Recently in November 2014, Jim retired.